Sepsis causes 1 death every 3-4 seconds2

In the next 5 minutes, approximately 75 people will die of sepsis globally2
- Sepsis is one of the leading causes of death globally6
- In the Western world 7,8, sepsis is one of the most expensive conditions
- 15-40% of patients receive inappropriate initial antimicrobial therapy12
- Speed counts – results in minutes vs. hours offers the potential to tailor initial antimicrobial therapy, which has shown to improve outcomes5
It's All About Time
Qvella’s FAST-Technology™ (Field Activated Sample Treatment) facilitates automation and acceleration of different stages of microbiology workflow to generate actionable information for bloodstream infections in minutes. FAST-Technology includes preferential lysis of sample cells, rapid isolation and concentration of specific target cell types including pathogenic cells, extraction-free, in-line e-Lysis™ producing a clean, NAAT-ready lysate.
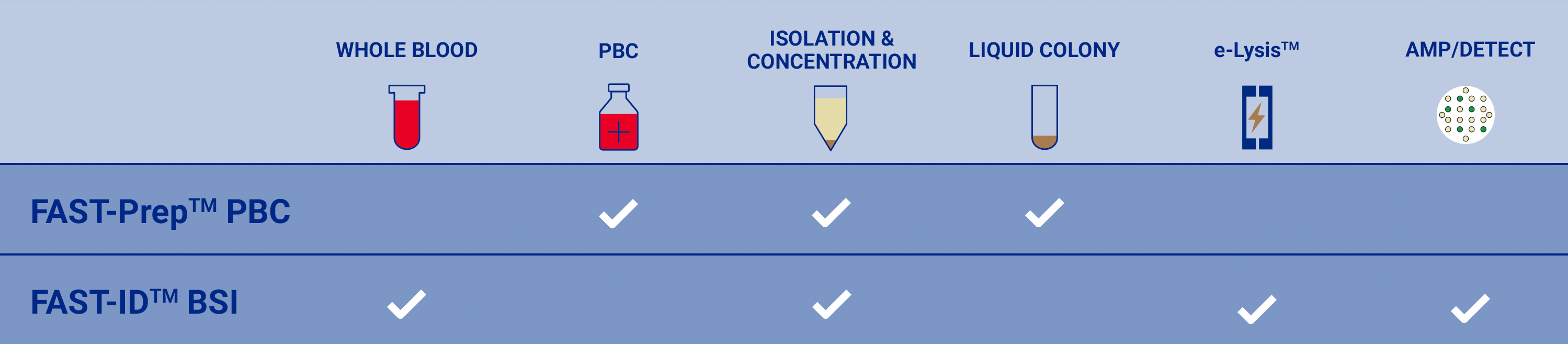
The FAST-PrepTM PBC System

The FAST-ID™ BSI System*

Designed to detect over 90% of pathogens causing Sepsis in less than one hour directly from blood
- Surviving Sepsis Campaign (SSC)10 and UK National Institute for Health and Care Excellence (NICE)11 guidelines call for antimicrobial therapy within 1 hour of diagnosis of sepsis
- Every hour of delay in appropriate initial antibiotic therapy increases mortality by 7.6% associated with severe sepsis5
- Designed for detection of mono- or poly-microbial bloodstream infections in less than an hour
- Results reported as 16 individual test results at either the family, genus or species level
¥ FAST-Prep™ PBC System is under development and not approved for sale. The performance characteristics have not been established. The system will not be validated for any specific downstream diagnostic applications, and use will only be indicated for positive blood cultures. The user will be responsible for validating the system in combination with diagnostic procedures used in their laboratory and in accordance with applicable regulations.
*FAST-ID™ is under development and not approved for sale. The performance characteristics have not been established.
1Sepsis Alliance (2016, November) Sepsis 2016 fact sheet Retrieved from https://www.sepsis.org/downloads/2016_sepsis_facts_media.pdf
2Dugani, S., Laxminarayan, R., & Kissoon, N. (2017). The quadruple burden of sepsis. Canadian Medical Association Journal, 189 (36), E1128-E1129.
3Fleischmann C. et al. (2016). Assessment of Global Incidence and Mortality of Hospital-treated Sepsis. Current Estimates and Limitations, Am J Respir Crit Care Med, 1;193(3), 259-72.
4National Inpatient Hospital Costs: The Most Expensive Conditions by Payer, 2013 (MAY 2016) HCUP Statistical Brief #204 Retrieved from https://www.hcup-us.ahrq.gov/reports/statbriefs/sb204-Most-Expensive-Hospital-Conditions.pdf
5Kumar et al. (2015). Empiric Antimicrobial Therapy in Severe Sepsis and Septic Shock: Optimizing Pathogen Clearance. Curr Infect Dis Rep.,17(7), 493.
6Global Sepsis Alliance (2015, September) Retrieved from http://www.wfpiccs.org/wp-content/uploads/2015/09/2015_WSD_FactSheet_long_English.pdf
7European Commission: CORDIS: Projects and Results: Next generation sepsis diagnosis. (2016) Retrieved from Cordis.europa.eu. http://cordis.europa.eu/project/rcn/199396_en.html
8National Inpatient Hospital Costs: The Most Expensive Conditions by Payer, 2013 #204. (2016, May) Retrieved from Hcup-us.ahrq.gov. https://www.hcup-us.ahrq.gov/reports/statbriefs/sb204-Most-Expensive-Hospital-Conditions.jsp
9Lueangarun, S. & Leelarasamee, A. (2012). Impact of Inappropriate Empiric Antimicrobial Therapy on Mortality of Septic Patients with Bacteremia: A Retrospective Study. Interdisciplinary Perspectives on Infectious Diseases, Volume 2012, Article ID 765205, 13.
10Andrew Rhodes et al. (2017). Surviving Sepsis Campaign: International Guidelines for Management of Sepsis and Septic Shock, Crit Care Med, 45(3), 486-552.
11National Institute for Health and Care Excellence Nice.org.uk (2017, September) Retrieved from https://www.nice.org.uk/guidance/qs161/chapter/Quality-statements
12McDonald et.al. (2005).Risk Factors for Ineffective Therapy in Patients with Bloodstream Infection, Arch Intern Med. 2005; 165308-313